There is a predicted shortage of 55,200 primary care physicians and 86,700 specialists by the year 2033 per a report by the Association of American Medical Colleges. The patient population is growing, especially in its aging population, and the number of physicians is not. This large shortfall needs to have a remedy now to prepare for that not-too-distant future. There are some trends in healthcare that may be to blame, and the future of medicine may be managed differently because of these trends.
Healthcare in general took a big hit during the pandemic with real-time media, internet, and social media bombarding the patients. As the pandemic was unfolding, and as the treatments and race for a vaccine strategy were unfolding there was so much information to sift through. The World Health Organization coined the term “infodemic” describing this period with unrestrained misinformation weaving between the viable information. I still have a hard time deciding what information was intentionally misleading versus that which rolled out, without editing, and became inaccurate because it simply was not properly vetted or thought through. I certainly have my opinions on what was true science versus that cloaked as true science, and of course, this created a big divide in the country. That said, the current trend in healthcare includes the vital need now to rebuild trust. Physicians at the helm of the medical decision-making will need to help patients gain access to evidence-based, trustworthy information. We physicians must be dutiful to this endeavor despite any pressures from entities outside of the physician-patient relationship. Hearsay will no longer be acceptable to information savvy patients.

Clearly trending is the patient-centered approach of functional and integrative care. Patients are also taking much more ownership of their personal health information. With such a push in these past two years to receive the newest in technology and that of mRNA vaccine technology, there was little information shared to the public about those action steps that a patient could take to remain well and to improve the immune system. The technologic bullet we manufactured did not consider those large sectors of low-risk patients who had strategies and genetics that made them resilient to end-stage disease. Functional medicine will certainly get at the very root of a person’s malady incorporating so many facets of evidence-based tests and treatments. However, these treatments may branch out into other sciences, yes sciences, to achieve the improvement. The functional model is built on four pillars as coined by Dr Jeffrey Bland that is: predictive, preventive, personalized, and participatory. Some of the principles are either lacking or not well supported in the current healthcare model. Think of yourself as a patient and whether you want to be valued and treated as unique, an active participant, and with tools that resonate with you. The functional tools are vast and include nutrition, movement, supplementation, psychology, spirituality, sleep, energy, and traditional approaches. Functional medicine also is very collaborative and invites the input from all disciplines of acupuncture, Eastern practitioners, chiropractors, energy workers, therapists, and spiritual leaders.
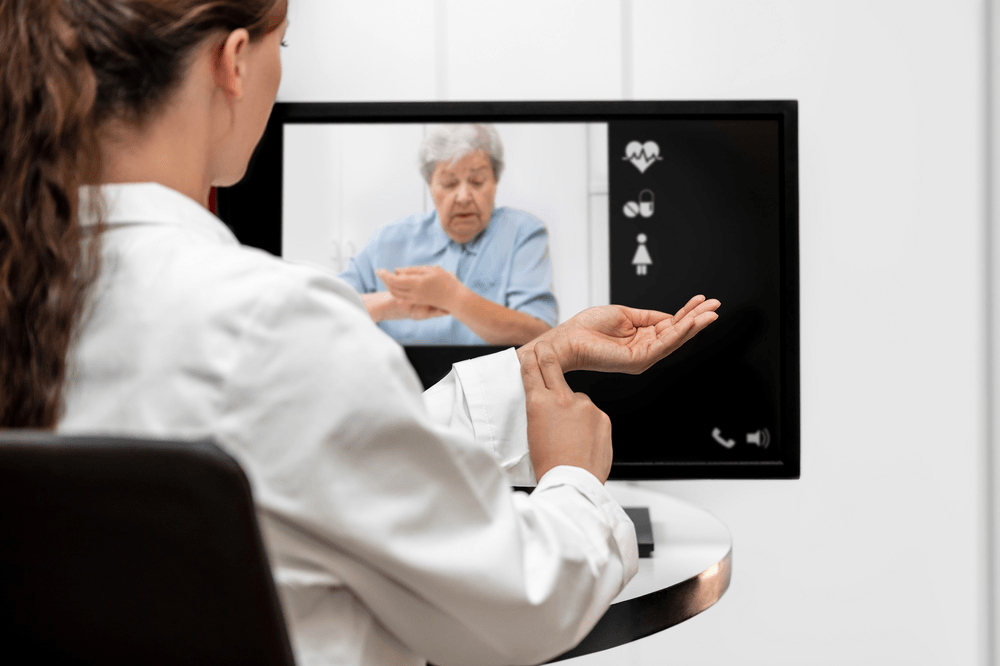
Technology and telemedicine platforms are rising exponentially. The visits are easy to conduct, and patients have the luxury of visits in their own comfortable environment. Telemedicine also allows patients to work around hectic schedules and family obligations. I believe that these platforms can capture more people that had previously no access to health care based upon work constraints, transportation, and childcare. Electronic recording has made prescribing very easy as well as documenting and billing. Many patients have mobile jobs, and this also is a way to keep a continuity of care. There are limitations, but even in the ever-evolving world of technology there are electronic blood pressure cuffs, medical photography, and monitoring systems to place in the home to essentially plug in the data to a health portal. Telemedicine combined with the functional medicine physician also can assure you of your specific doctor rather than seeing whoever is on duty.
Healthcare spending continues to climb. This is not a favorable trend, and sadly, over the past ten years, medical bills are the number one cause of bankruptcies nationwide. With affordable care acts and Medicaid subsidies, there are more patients insured. Many choose high deductible plans in hope that the lowered premium is enough to insure themselves. However, many people skip medical care to avoid the high cost of that high deductible co-pay. Because of the climbing healthcare costs, we see the rise of health share plans. Health share plans are not traditional insurance, but they do qualify as insurance as defined in the Affordable Care Act. Costs are lower per month and patients “share” expenses throughout the group. Most time if the physician or health system doesn’t participate with the sharing plan, the patient pays up front but gets reimbursed by the plan. I’ve seen these plans work fluidly for families in my functional practice.
Trending in the past two years and bringing it to the forefront is physician burnout. I’ve often said that I wore workaholism as a badge in my career. Currently, 70% of physicians would not recommend healthcare as a career. Physicians really need to balance the professional career with family and a personal life. I can attest that I did not always do that in a harmonic balance. As the electronic health systems and the merging of practices into large health systems, workload has increased. Workload and the operational flow are at the heart of burnout issues with little or no ability to affect change. Certainly, in the pandemic many were burning out because of anxieties revolving around the “second surge” and “crisis fatigue.” We physicians also fell victim to societal issues outside of the office with social justice and politics. We tried to lead with a lot of oppression to overcome, and after a while it took its toll. Physicians are retiring early. What I am foreseeing, however, is the private practice sector gaining traction again. The family doctor who was at the core of the community may be making a comeback. I had a wise mentor once tell me that medicine comes in waves, and perhaps we are cycling back to the wave of your personal doctor, with personalized medicine, with the new spin of technology creating more rewarding and easier visits. I look forward to this.






Comments are closed.